

Improving Health Care in Malawi
In rural, low-resource communities, access to health care can be challenging. The next concern is the quality of that care.
“High-quality health care shouldn’t be accessible only to people who have money to pay. Everyone deserves high-quality care,” says Chikumbutso Lester, chairperson of the quality improvement team, Mlale Mission Hospital in Lilongwe, Malawi.
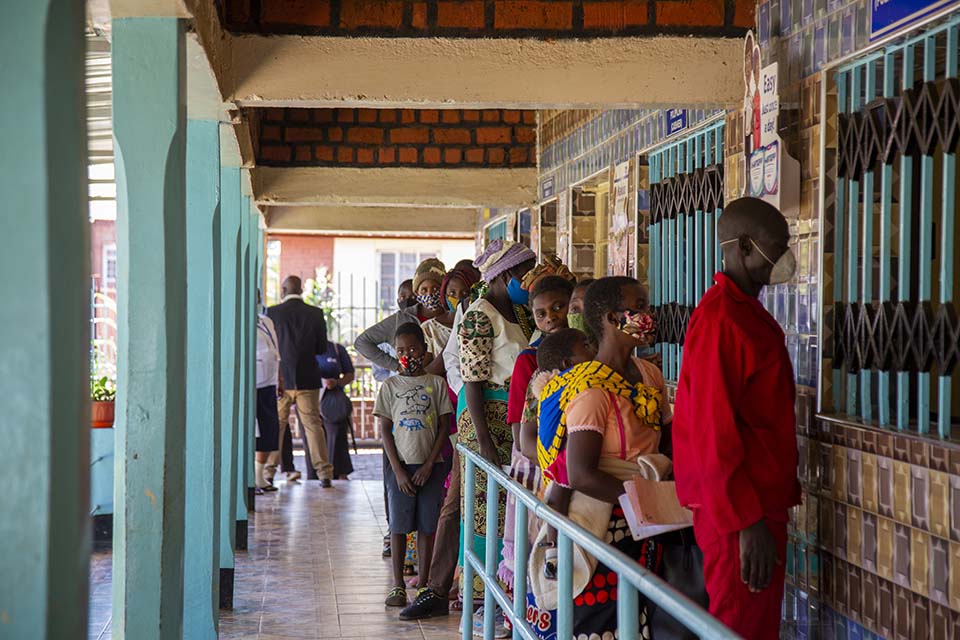
Patients at Mlale Mission Hospital in Lilongwe, Malawi. The CRS SAFECARE project worked with the hospital to improve the quality of their health care service delivery by 16 percentage points.
Photo: Dooshima Tsee/CRS
When patients go to a hospital, they are often at their most vulnerable. They must trust that the facility has the right processes and amenities to provide the services they need to recover.
In sub-Saharan Africa, health facilities grapple with increasing pressure from a growing population, limited financial resources, emerging infectious diseases like COVID-19 and increasing numbers of people suffering from non-communicable chronic diseases. These challenges can often stress health facilities trying to provide reliable, consistent quality health services.
Trust is a crucial component in keeping communities healthy and eliminating disparities in health, especially in low-resource or underserved communities. Catholic Relief Services is helping faith-based health facilities in Malawi be more responsive to the growing and changing needs of the patients in their communities.
The United Nation’s Sustainable Development Goals stress that quality is a key element of universal health coverage, including financial risk protection alongside access to quality essential health care services for all. CRS is helping to ensure that people get access to the highest quality of care from the health facilities closest to them. This is crucial to achieving more equitable health care.
“The first hour when a patient arrives at the hospital is very important. What happens in that first hour can sometimes be the difference between life and death,” says Airedi Zabuloni-Kwakwala, the nurse in charge of the outpatient department at Mlambe Mission Hospital in Lunzu, Malawi.

Airedi Zabuloni-Kwakwala is the nursing officer in charge of the outpatient department and emergency room in Lunzu, Blantyre District, Malawi. Reorganizing the department helps save lives in the fast-paced hospital settings.
Photo: Dooshima Tsee/CRS
Mlambe Mission Hospital is a Catholic hospital managed by the Daughters of Wisdom. Zabuloni‑Kwakwala joined the hospital staff in April 2020. She came with a wealth of knowledge from working in a much larger hospital and managing an outpatient and emergency department for over five years in the nation’s capital. This experience was valuable when Mlambe Mission Hospital was reorganizing their outpatient set up.
As the hospital’s administrator, Felix Chauluka’s job is to make sure the entire facility runs smoothly. Reorganizing the outpatient department is only part of a much larger, long-range plan to improve the quality of health services at the hospital.
For decades, CRS has worked with national governments globally to strengthen health care systems. In 2019, CRS started working with faith-based hospitals across Malawi to help them work within internationally recognized health care standards and provide high-quality services to people in low resource, rural communities.
CRS uses the SafeCare method designed by PharmAccess to do this work. The method has several steps. It starts with assessing each facility to identify gaps in internationally accredited quality of care standards and measurable criteria.

Memory Mkandawire (nursing officer in charge of pediatrics) in the pediatric ward at Mlale Mission hospital in Lilongwe rural, Malawi.
Photo: Dooshima Tsee/CRS
Assessed facilities are certified from levels one to five. At level one, facilities are at risk of unsafe situations. At level five, treatment guidelines are regularly monitored and the highest quality of care standards are consistently sustained.
After the assessment, program teams work with the facility to develop annual quality improvement plans that get facilities started on their journey of continuous quality improvement. CRS delivers this program in partnership with the Episcopal Conference of Malawi. Both CRS and staff from the conference provide monthly virtual support calls to share quality improvement project experiences, and quarterly follow-up visits to facilities. The aim is to help facilities achieve self-sustainability and develop a culture of continuous quality improvement.
Felix says the continuous improvement process takes some of the decision-making power off his plate. The plan recognizes that staff who work in departments have intimate knowledge of how things work in their units and are in the best position to recommend improvements.
“The improvement protocols empowered people working in departments to make improvements that might not necessarily even cost money,” Felix says. “In the human resources department, for instance, one of the biggest changes we made was making and following checklists to ensure records are up to date.”
A couple hundred miles away in Mlale Mission Hospital, Sister Mini Thomas, the hospital administrator, agrees that knowing what to change is vital to improving.
“Most of us come into this work because it is our calling. We want to do what is best for the patients. It becomes difficult when you do not know what to do to improve. Knowing what to do to improve health services for patients was the biggest change for me,” Sister Mini says.

Health care workers and patients meet in a hallway in Mlambe hospital in Lunzu, Blantyre District, Malawi.
Photo: Dooshima Tsee/CRS
At their initial assessment in June 2019, Mlale hospital scored 39%. This placed them on level two of the grading system. Their individualized quality improvement plan listed several changes they could make. Over the next 24 months, they improved governance and management processes, human resource management, support services and risk management. Their score increased to 55% after another assessment in May 2021, which was delayed due to COVID-19 pandemic).
The change Sister Mini and her team made that had the most significant impact was how they restructured the intake process and the flow of patients that arrive at the hospital. Before, the intake process was inefficient and confusing. Patients were often unsure where to go and had to loop back across the hospital several times because touchpoints were not efficiently planned.
Now they have partitioned and reassigned rooms for efficiency. The reception area, accounts office, pharmacy and consulting rooms are now in the same vicinity. Patients move from one service to the other in logical sequence. Improved patient flow saves time for both clients and health staff. Overall, patients receive medical care more quickly, spend less time in the hospital and health care staff can attend to more patients.
Another major change was to the laundry sorting and waste disposal. Anness Thumba has worked in the laundry facilities at the hospital for over 26 years. Thumba and one other laundry worker sort and clean medical linen using disease prevention protocols. After training, they restructured the laundry room so contaminated linen never comes in contact with clean linen. The restructuring helps Thumba do her job better.

Anness Thumba hangs hospital linen in the sun to dry. Anness is a laundry worker at Mlale Mission Hospital in Lilongwe, Malawi.
Photo Dooshima Tsee/CRS
“I believe my job is important because it is part of preventive and healing measures for the hospital. Patients and staff have clean linen that smells good and is free from disease,” Anness says.
George Lipenga is also proud of his job disposing of medical waste. He manages waste disposal for both infectious medical waste and general hospital waste. He works hand in hand with the nurses and clinicians to properly segregate and dispose of waste.
Anness and George may not be on the front lines like doctors and nurses are. Still, they form an essential bulwark to prevent infections from spreading within the hospital and out to the surrounding community.

George Lipenga sorting hazardous waste in front of the waste sorting shelf used to manage waste at Mlale Mission Hospital in Lilongwe, Malawi.
Photo: Dooshima Tsee/CRS
There is still a lot of work to do. Teams at both hospitals are excited to make more changes because they can already see the positive effects of the previous quality improvement work. They believe they have the skills and support to make meaningful changes.
“It is not easy to change a process, especially if you have been doing things one way for a long time. But all of our staff are willing to try if it means better services for the patients.” —Anna Balley, matron and principal nursing officer, in her office at Mlambe Mission Hospital in Lunzu, Blantyre District, Malawi.
Anna Balley, principal nursing officer at Mlambe Mission Hospital, already knows the next round of changes to take place. One change is translating medical consent forms to local languages so patients can better understand and give informed consent for procedures.
Improving health care services and ensuring patients receive the highest quality of care—no matter where they are in the world—helps save lives. Refining behind-the-scenes processes, like laundry management, waste disposal and efficient patient intake, as well as more public-facing aspects of health care like reorganizing systems within an outpatient department, make high-quality universal health coverage more accessible to all.

